Imagine living in a country where access to healthcare is a fundamental right, where medical expenses are not a burden, and where everyone receives the care they need when they need it. Unfortunately, this utopian vision seems far-fetched in the current state of healthcare in the US. The nation’s healthcare system is broken, plagued by exorbitant costs, limited access, and disparities in quality. From insurance complexities to inflated drug prices, navigating the labyrinthine healthcare landscape can be an overwhelming and frustrating experience. It’s time to delve deeper into the cracks of this broken system, understand its intricacies, and explore potential solutions for a healthier future.
High costs of healthcare
Lack of price transparency
One of the major challenges facing the US healthcare system is the lack of price transparency. When seeking medical treatment, it can be incredibly difficult to determine the cost of a procedure or even a basic doctor’s visit. This lack of transparency leaves patients uncertain and uninformed about the financial implications of their healthcare decisions. Without the ability to compare prices, individuals are unable to make cost-effective choices and may unknowingly be charged exorbitant fees for the same services available elsewhere at a fraction of the cost.
Rising insurance premiums
Another significant concern is the rising cost of insurance premiums. Many Americans struggle to afford adequate healthcare coverage due to the ever-increasing premiums demanded by insurance companies. This creates a daunting financial burden, especially for individuals and families with limited incomes. As insurance premiums continue to rise, more and more people are forced to make difficult decisions regarding their healthcare, often having to sacrifice necessary treatments or preventive care due to cost constraints.
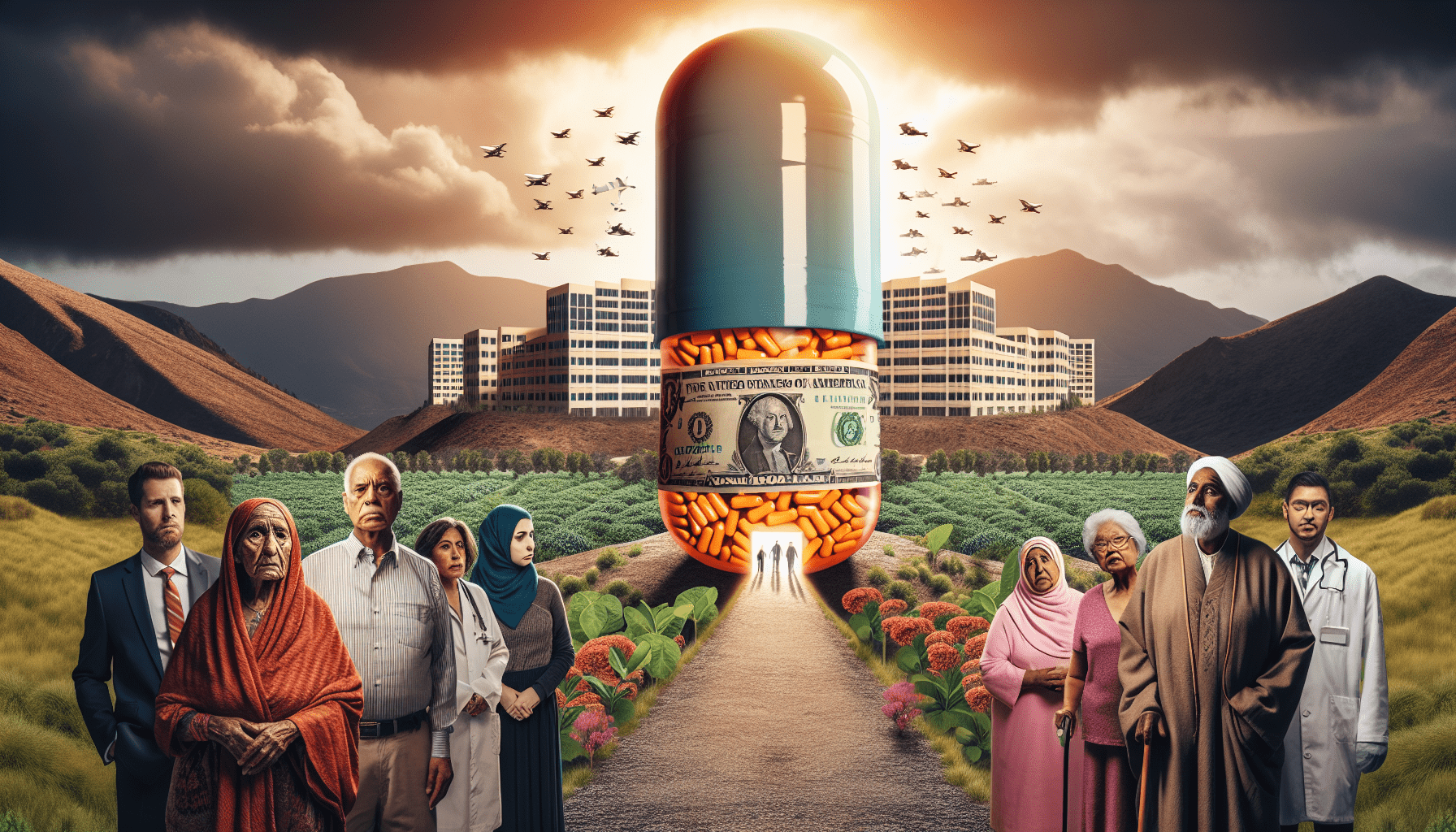
Expensive prescription medications
The exorbitant prices of prescription medications also contribute to the high costs of healthcare in the US. It is not uncommon for individuals to struggle with the affordability of life-saving medications, forcing them to choose between their health and financial stability. Pharmaceutical companies often prioritize profits over patient well-being, resulting in inflated prices that place an unfair burden on those in need of medication. This issue further highlights the brokenness of the healthcare system, as access to essential treatments becomes dependent on financial means rather than medical necessity.
Inadequate access to healthcare
Millions of uninsured individuals
A significant problem within the US healthcare system is the high number of uninsured individuals. According to recent statistics, millions of Americans remain without health insurance, leaving them vulnerable and unable to seek necessary medical care. This lack of coverage not only jeopardizes individual health but also places strain on the overall healthcare system, as untreated conditions can escalate and require more intensive and expensive care. Providing accessible and affordable healthcare coverage for all should be a priority in order to ensure equitable care for everyone.
Limited availability of healthcare providers
Even for those with health insurance, access to healthcare providers can be limited. Certain specialties and services often experience shortages, resulting in long wait times for appointments and delayed treatment. This lack of available providers puts unnecessary strain on patients, forcing them to endure increased discomfort or risk worsening health conditions while they wait for care. Overall, the insufficient number of healthcare providers poses a significant barrier to timely and accessible healthcare for many Americans.
Healthcare deserts in rural areas
One particular concern regarding access to healthcare is the presence of healthcare deserts in rural areas. These are regions where residents have limited access to healthcare facilities due to geographic or logistical constraints. Rural communities often face challenges in attracting and retaining healthcare professionals, leading to insufficient healthcare options for their residents. As a result, individuals in these areas may have to travel long distances to receive necessary medical care, further exacerbating the already existing healthcare disparities between urban and rural populations.
Inequity in healthcare
Healthcare disparities based on socioeconomic factors
In the US healthcare system, there are significant healthcare disparities based on socioeconomic factors. Individuals from marginalized communities or lower-income backgrounds often face unequal access to quality healthcare. This inequality perpetuates a cycle of poor health outcomes and limited opportunities for individuals to improve their well-being. Socioeconomic factors such as income, education, and race should not determine the level of healthcare a person receives. Addressing these disparities and striving for equitable healthcare provision is crucial for building a fair and just healthcare system.
Unequal access to quality healthcare for marginalized populations
Marginalized populations, including racial and ethnic minorities, immigrants, and the LGBTQ+ community, often face barriers to accessing quality healthcare. Discrimination, biases, and cultural incompetency within the healthcare system can lead to subpar care and inadequate attention to their unique health needs. Improving access and eliminating barriers for marginalized populations is essential to ensure that every individual receives the care they deserve, regardless of their background or identity.
Fragmented healthcare system
Lack of coordination among healthcare providers
The US healthcare system suffers from a lack of coordination among healthcare providers. Patients navigating through different healthcare settings often encounter difficulties in receiving seamless and integrated care. Fragmentation of care can lead to disjointed treatment plans, miscommunication between healthcare professionals, and unnecessary repetition of tests or procedures. To address this issue, enhanced coordination and communication between healthcare providers are necessary, facilitating a more efficient and effective healthcare experience for patients.
Difficulty transitioning between different healthcare settings
Transitioning between different healthcare settings, such as hospitals, outpatient clinics, and home care, can present challenges for patients. Inadequate coordination and communication during these transitions can result in gaps in care, medical errors, and confusion for patients and their families. Establishing standardized protocols and systems to ensure smooth transitions and continuity of care is critical in providing a cohesive healthcare experience, especially for individuals with complex or chronic conditions that require ongoing management.

Emphasis on profit over care
Pharmaceutical companies prioritizing profits over patient well-being
An area of concern within the US healthcare system is the focus on profit over patient well-being by pharmaceutical companies. The rising costs of prescription medications often stem from the pursuit of financial gain rather than the genuine concern for improving health outcomes. This emphasis on profit forces individuals to bear the burden of exorbitant drug prices, leading to financial hardships and limited access to essential medications. Shifting the focus towards patient well-being and affordability is crucial to ensure that life-saving treatments are accessible to all who need them.
Health insurance companies focusing on financial gains
Similarly, health insurance companies sometimes prioritize financial gains over the well-being of their policyholders. The rising insurance premiums mentioned earlier are often driven by the profit-seeking motives of these companies. This can result in limited coverage, high deductibles, and complex reimbursement processes, leaving individuals struggling to navigate the intricacies of their insurance plans. Reevaluating the priorities of health insurance companies to prioritize affordable coverage and comprehensive care would go a long way in alleviating the financial burden on patients and improving the overall quality of healthcare.
Medical debt crisis
Large number of individuals facing medical bankruptcy
The high costs of healthcare in the US contribute to a medical debt crisis, with a significant number of individuals and families facing medical bankruptcy. The burden of medical debt can be overwhelming, forcing individuals to make difficult choices between paying medical bills and meeting other basic needs. This level of financial strain not only affects the individuals directly but also has broader economic implications as families struggle to recover financially. Addressing the root causes of medical debt and implementing measures to mitigate its impact is crucial in building a more sustainable and equitable healthcare system.
Financial burden on patients due to high healthcare costs
Apart from the risk of medical bankruptcy, the high healthcare costs place a significant financial burden on patients. Even with health insurance, individuals often face substantial out-of-pocket expenses in the form of deductibles, co-pays, and uncovered services. These costs can quickly add up, leaving individuals in a state of financial stress and potentially deterring them from seeking necessary care. Ensuring affordable healthcare options and reducing the out-of-pocket expenses for individuals is vital to alleviate the financial strain and promote equitable access to healthcare.

Lack of preventive care
Insufficient emphasis on preventive measures
The US healthcare system tends to focus on reactive rather than proactive healthcare approaches, placing insufficient emphasis on preventive measures. Preventive care plays a crucial role in maintaining overall health and well-being, as it can help identify and address health issues before they progress and become more severe. However, without proper emphasis and support for preventive care, individuals may delay or forgo necessary screenings, immunizations, and other preventive interventions, leading to higher healthcare costs and poorer health outcomes in the long run.
Focus on reactive rather than proactive healthcare approach
The reactive approach to healthcare in the US means that many individuals seek medical attention only when they experience symptoms or when their health conditions have already worsened. This approach often leads to delayed diagnoses, more intensive treatments, and higher healthcare costs. Shifting towards a more proactive healthcare approach that encourages regular check-ups, preventive screenings, and health education would not only improve overall health outcomes but also reduce healthcare expenditures in the long term.
Inefficiencies in healthcare delivery
Burdensome administrative tasks
Healthcare providers often face burdensome administrative tasks that detract from their ability to focus on patient care. Complex billing and reimbursement processes, excessive paperwork, and regulatory requirements consume valuable time and resources. The administrative burden placed on healthcare professionals can negatively impact their job satisfaction and contribute to physician burnout, ultimately affecting the quality of care provided. Streamlining administrative processes and reducing unnecessary paperwork would allow healthcare providers to devote more time and attention to patient care, leading to improved healthcare experiences for all.
Redundant paperwork and documentation
The US healthcare system is notorious for its redundant paperwork and documentation requirements. Patients often have to fill out the same forms repeatedly and provide duplicate information to multiple healthcare providers. This not only creates frustrations for patients but also leads to inefficiencies in the system. Transitioning towards more streamlined electronic medical records and standardized documentation processes would not only save time and resources but also enhance patient experiences by minimizing duplicate paperwork and ensuring accurate medical information across different healthcare settings.
Long wait times for medical appointments
Long wait times for medical appointments have become a common frustration for many patients in the US. Whether it’s scheduling routine check-ups or obtaining specialized care, the wait times can be extensive, resulting in delayed diagnoses and treatment. Long wait times can also be a barrier to accessing timely care, potentially compromising patient outcomes. Increasing the number of healthcare providers, optimizing scheduling systems, and exploring virtual care options can help reduce wait times and improve access to timely healthcare services, ensuring that patients receive the care they need when they need it.
Quality of care concerns
Medication errors and preventable medical mistakes
Quality of care concerns within the US healthcare system include medication errors and preventable medical mistakes. These errors can have severe consequences for patients, potentially leading to adverse reactions, prolonged hospital stays, or even fatalities. Focusing on patient safety and implementing comprehensive measures to prevent and mitigate medication errors and medical mistakes is vital to ensure that healthcare providers deliver high-quality care that patients can trust.
Variability in healthcare outcomes
Variances in healthcare outcomes across different providers and regions are another pressing quality of care concern. Quality should not be a matter of chance or geographic location, but rather a fundamental right for all individuals. Addressing the variability in outcomes requires implementing standardized best practices, fostering knowledge sharing among healthcare providers, and holding healthcare organizations accountable for delivering consistently high-quality care. By doing so, patients can have confidence in the care they receive regardless of where they seek treatment.
Inadequate patient education and communication
A crucial aspect of quality care is effective patient education and communication. However, the US healthcare system often falls short in providing patients with adequate information and involving them in their care decisions. Inadequate patient education can lead to misunderstandings, non-compliance with treatment plans, and suboptimal health outcomes. Improving patient education and communication within healthcare settings, including clear explanations of diagnoses, treatment options, and potential risks, empowers patients to actively participate in their own care, ultimately leading to better health outcomes and increased patient satisfaction.
Sustainable healthcare solutions
Promotion of universal healthcare coverage
A sustainable solution to the broken US healthcare system is the promotion of universal healthcare coverage. By ensuring that every individual has access to comprehensive and affordable healthcare, the disparities and inequities in care can be significantly reduced. Universal healthcare would remove the financial barriers associated with seeking medical treatment, saving individuals from the burden of medical debt and bankruptcy. Moreover, it would foster a healthier population overall, with increased focus on preventive care and early intervention, leading to improved health outcomes and reduced healthcare costs in the long run.
Value-based healthcare delivery models
Another potential solution lies in transitioning towards value-based healthcare delivery models. Instead of the current fee-for-service approach, value-based models prioritize patient outcomes and the quality of care provided. These models incentivize healthcare providers to deliver efficient, effective, and patient-centered care, aligning financial incentives with the overall well-being of patients. By shifting the focus from quantity to quality, value-based healthcare models can drive improvements in care delivery and promote better health outcomes for individuals and communities.
Investment in healthcare workforce and infrastructure
Investing in the healthcare workforce and infrastructure is crucial in building a sustainable healthcare system. This includes increasing the number of healthcare professionals, improving their training and education, and ensuring adequate staffing ratios in healthcare settings. Additionally, investments in healthcare infrastructure, such as technology advancements and the development of telehealth capabilities, can enhance the delivery of care, particularly in underserved areas. By prioritizing these investments, the US healthcare system can address many of its existing challenges and effectively meet the healthcare needs of its population.
In conclusion, the US healthcare system is facing multiple challenges that contribute to its broken state. From high costs and inadequate access to inequities and fragmented care, the system is in dire need of comprehensive reform. Addressing these issues requires a multifaceted approach that tackles the root causes of inefficiencies and disparities. By prioritizing transparency, equity, and quality, while also promoting preventive care and sustainable solutions, the US can work towards a healthcare system that provides accessible, affordable, and high-quality care for all.

