Arthritis, a condition that affects millions of people worldwide, has long been a subject of scientific investigation. In recent years, researchers have turned their attention to understanding the role of genetic factors in the development of arthritis. This article explores the fascinating world of genetics and how certain factors contribute to the onset of this debilitating condition. By unraveling the intricate relationship between genes and arthritis, scientists hope to pave the way for more effective treatments and preventive measures.
Overview of Arthritis
Definition of arthritis
Arthritis is a medical condition characterized by inflammation and stiffness in the joints, which can result in pain and reduced mobility. There are many different types of arthritis, each with its specific symptoms and underlying causes. It is a chronic condition that affects millions of people worldwide.
Types of arthritis
There are more than 100 types of arthritis, but the most common ones include osteoarthritis, rheumatoid arthritis, psoriatic arthritis, gout, and spondyloarthritis. Each type has distinct characteristics and affects different joints in the body.
Prevalence of arthritis
Arthritis is a prevalent condition, with approximately 350 million people worldwide affected by it. It can occur in people of all ages, although it is more common among older individuals. The prevalence varies depending on the type of arthritis, with osteoarthritis being the most common form among adults.
Impact of arthritis on daily life
Arthritis can have a significant impact on daily life. The pain, stiffness, and reduced mobility associated with the condition can make it challenging for individuals to engage in activities they once enjoyed. Simple tasks like walking, dressing, or cooking may become difficult, leading to decreased independence and a lower quality of life. It is essential to manage arthritis effectively to minimize its impact on daily activities.
Understanding Genetics
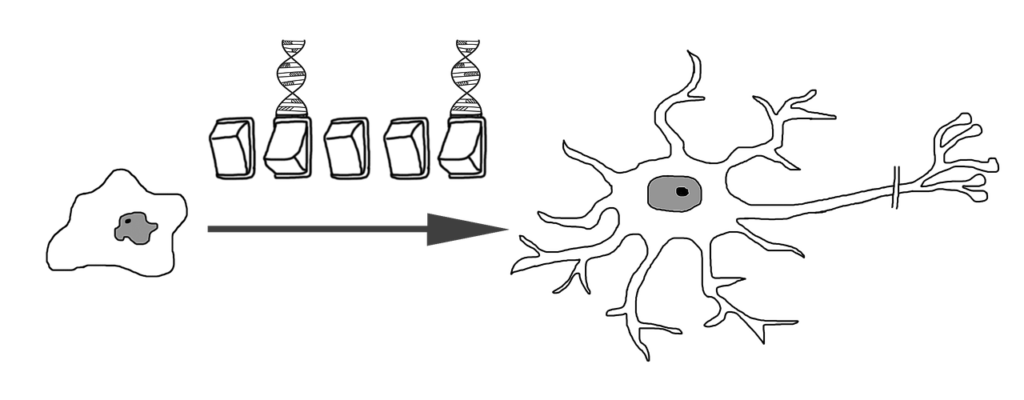
Basics of genetics
Genetics is the study of genes and how they are passed down from parents to offspring. Genes are segments of DNA that carry the instructions for specific traits and characteristics. They determine everything from eye color to susceptibility to certain diseases.
The role of genes
Genes play a critical role in the development and functioning of the human body. They influence various aspects, including physical appearance, metabolism, and the immune system. Certain genes are also associated with an increased risk of developing certain diseases, including arthritis.
Genetic variations and mutations
Genes can have variations or mutations, which can result in differences in traits or an increased susceptibility to diseases. These variations can occur naturally or be inherited from parents. The study of genetic variations helps researchers understand the underlying causes of diseases and their potential treatment strategies.
Inheritance patterns
Genes are passed down from parents to their children in specific patterns. These inheritance patterns can vary depending on the type of trait or disease being inherited. In the case of arthritis, certain genetic factors are known to have a hereditary component, making individuals more susceptible to developing the condition if they have a family history.
Genetic Factors and Arthritis
Genetic predisposition
Genetic predisposition refers to an increased susceptibility of an individual to develop a particular disease or condition based on their genetic makeup. In the case of arthritis, certain genetic factors can contribute to an individual’s increased risk of developing the disease. However, having these genetic factors does not guarantee that a person will develop arthritis, as other environmental and lifestyle factors also play a role.
Linkage studies
Linkage studies are a type of genetic study that examines the inheritance pattern of specific genetic markers or variations within families. These studies aim to identify potential genetic regions or genes associated with a particular disease or trait. In the context of arthritis, linkage studies have helped researchers identify several genetic factors linked to its development.
Candidate gene studies
Candidate gene studies focus on specific genes that are known or suspected to play a role in a particular disease. Researchers choose these genes based on previous knowledge or biological plausibility. By studying these candidate genes in individuals with arthritis, researchers can better understand the link between genetics and the development of the disease.
Genome-wide association studies (GWAS)
Genome-wide association studies (GWAS) examine the entire genome of individuals to identify genetic variations associated with a particular disease. These studies involve analyzing genetic differences between individuals with and without the disease, aiming to understand the specific genes or areas of the genome contributing to disease susceptibility. GWAS have played a crucial role in identifying numerous genetic factors associated with arthritis.
Major Genetic Factors Associated with Arthritis
HLA genes
The human leukocyte antigen (HLA) genes are a group of genes related to the immune system’s functioning. These genes are responsible for presenting foreign substances to the immune system, triggering an immune response. Certain variations in the HLA genes have been strongly linked to several types of arthritis, including rheumatoid arthritis and ankylosing spondylitis.
PTPN22 gene
The PTPN22 gene is involved in regulating the immune system’s activity, particularly in autoimmune diseases. Variations in this gene have been linked to an increased risk of developing rheumatoid arthritis and other autoimmune diseases. The specific variant associated with arthritis can affect immune responses, leading to an abnormal attack on the body’s tissues.
IL6 gene
The IL6 gene codes for a protein called interleukin-6, which plays a crucial role in inflammation and immune responses. Variations in the IL6 gene have been associated with an increased risk of developing rheumatoid arthritis and systemic juvenile idiopathic arthritis. Research into the IL6 gene’s role in arthritis has led to the development of targeted therapies that block the IL6 receptor.
IL1B gene
The IL1B gene is responsible for producing the protein interleukin-1 beta, which is involved in the inflammatory response. Variations in this gene have been linked to an increased susceptibility to rheumatoid arthritis and osteoarthritis. Understanding the role of the IL1B gene in arthritis has paved the way for potential therapeutic strategies targeting the IL1B pathway.
TNF gene
The TNF gene codes for the protein tumor necrosis factor-alpha (TNF-alpha), which plays a critical role in inflammation. Variations in the TNF gene have been associated with an increased risk of developing rheumatoid arthritis and psoriatic arthritis. Anti-TNF therapies, which block the activity of TNF-alpha, have emerged as an effective treatment option for these types of arthritis.
Role of HLA Genes in Arthritis Development
HLA gene complex
The HLA gene complex is a region on chromosome 6 that contains a group of genes responsible for regulating the immune system. These genes produce proteins that play a crucial role in recognizing and eliminating foreign substances. Variations in the HLA gene complex have been strongly associated with several immune-mediated diseases, including different types of arthritis.
Different HLA gene variants
Within the HLA gene complex, there are numerous variants or alleles that can be inherited from parents. Certain HLA gene variants, such as HLA-DRB1 in rheumatoid arthritis and HLA-B27 in spondyloarthritis, have been consistently linked to an increased risk of developing these specific types of arthritis. These gene variants influence the immune response and contribute to the development of the disease.
Association with different types of arthritis
HLA gene variants have been associated with various types of arthritis. For example, HLA-DRB1 variants, specifically the shared epitope, are strongly associated with rheumatoid arthritis. On the other hand, the HLA-B27 variant is associated with an increased risk of developing spondyloarthritis, including ankylosing spondylitis and reactive arthritis. The presence of these gene variants helps identify individuals at a higher risk of developing these specific types of arthritis.
HLA-B27 and its association with spondyloarthritis
The HLA-B27 gene variant is strongly associated with spondyloarthritis, a group of inflammatory diseases affecting the spine and joints. Having the HLA-B27 variant increases an individual’s susceptibility to developing spondyloarthritis, although not all individuals with the variant will develop the disease. The presence of HLA-B27 is often used as a diagnostic tool for spondyloarthritis.
PTPN22 Gene and Arthritis
Function of PTPN22 gene
The PTPN22 gene encodes a protein tyrosine phosphatase called LYP. This protein is involved in regulating immune cell function and preventing excessive immune responses. However, variations in the PTPN22 gene can impair its normal function, leading to an abnormal immune response and potentially contributing to the development of autoimmune diseases such as rheumatoid arthritis.
Association with rheumatoid arthritis
Variations in the PTPN22 gene have been strongly associated with an increased risk of developing rheumatoid arthritis. The specific variant, known as the 1858T allele, affects immune cell signaling and responsiveness. Individuals with this variant are more likely to develop rheumatoid arthritis, and the presence of the variant may also influence disease severity and treatment response.
PTPN22 variant and autoimmune response
The PTPN22 variant associated with rheumatoid arthritis can lead to an impaired regulation of immune responses. It affects the activation and function of T cells, B cells, and other immune cells, leading to an abnormal autoimmune response and the development of arthritis.
Impact on disease severity and treatment response
The presence of the PTPN22 variant has been found to be associated with increased disease severity in rheumatoid arthritis. Individuals with the variant may experience more aggressive disease progression, joint damage, and higher levels of inflammation. Additionally, studies have shown that the PTPN22 variant can influence the response to certain rheumatoid arthritis treatments, highlighting the importance of genetic factors in individual treatment outcomes.

IL6 Gene and Arthritis
Role of IL6 in inflammation
Interleukin-6 (IL6) is a cytokine produced by immune cells and other tissues in response to inflammation. It plays a crucial role in promoting inflammation but can also have beneficial effects in regulating the immune response. IL6 is involved in the activation and proliferation of immune cells and contributes to the production of other inflammatory molecules.
Association with rheumatoid arthritis and systemic juvenile idiopathic arthritis
Variations in the IL6 gene have been associated with an increased risk of developing rheumatoid arthritis and systemic juvenile idiopathic arthritis (SJIA). The specific gene variants affect IL6 production, leading to abnormal levels of the cytokine. These elevated levels can contribute to chronic inflammation and the development of arthritis in susceptible individuals.
IL6 receptor blockers as targeted therapy
The association between IL6 gene variants and arthritis has led to the development of targeted therapies that block the IL6 receptor. Monoclonal antibodies, such as tocilizumab, can bind to the IL6 receptor and inhibit its activation, thereby reducing inflammation. These IL6 receptor blockers have shown promising results in treating rheumatoid arthritis and SJIA.
IL6 gene polymorphisms and disease susceptibility
Different variations in the IL6 gene can modulate an individual’s susceptibility to rheumatoid arthritis and SJIA. Some variants have been associated with an increased risk of developing the diseases, while others may have a protective effect. The study of IL6 gene polymorphisms provides insights into the underlying mechanisms of these diseases and offers potential targets for future therapeutic interventions.
IL1B Gene and Arthritis
IL1B and its role in inflammation
Interleukin-1 beta (IL1B) is a pro-inflammatory cytokine produced primarily by immune cells. It is involved in the initiation and amplification of the inflammatory response and contributes to tissue damage in chronic inflammatory diseases. IL1B plays a critical role in the pathogenesis of various arthritis types, including rheumatoid arthritis and osteoarthritis.
Association with osteoarthritis and rheumatoid arthritis
Variations in the IL1B gene have been associated with an increased risk of developing both osteoarthritis and rheumatoid arthritis. These gene variants affect IL1B production and activity, leading to higher levels of inflammation and an increased susceptibility to arthritis. Understanding the role of the IL1B gene in arthritis provides valuable insights into disease mechanisms and potential therapeutic targets.
IL1B gene variants and disease severity
Certain IL1B gene variants have been associated with increased disease severity in arthritis. They have been linked to more extensive joint damage, increased pain, and a higher risk of complications. These gene variants play a role in shaping the clinical manifestations of arthritis and may help predict disease outcomes.
Therapeutic strategies targeting IL1B pathway
The association between IL1B gene variants and arthritis has opened up avenues for therapeutic strategies targeting the IL1B pathway. Drugs that inhibit IL1B, such as IL1 receptor antagonists and monoclonal antibodies, have shown efficacy in reducing inflammation and improving symptoms in patients with arthritis. These targeted therapies offer a more specific approach to treating the underlying cause of the disease.
TNF Gene and Arthritis
TNF and its role in inflammation
Tumor necrosis factor-alpha (TNF-alpha) is a pro-inflammatory cytokine involved in triggering and amplifying the inflammatory response. It plays a crucial role in the pathogenesis of various arthritis types, including rheumatoid arthritis and psoriatic arthritis. TNF-alpha contributes to joint inflammation, tissue damage, and the production of other inflammatory molecules.
Association with rheumatoid arthritis and psoriatic arthritis
Variations in the TNF gene have been associated with an increased risk of developing rheumatoid arthritis and psoriatic arthritis. These gene variants affect TNF-alpha production and activity, leading to chronic inflammation and the development of arthritis. The association between TNF gene variants and arthritis has led to significant advancements in treatment options.
Anti-TNF therapies for arthritis
Targeted therapies that block TNF-alpha activity have revolutionized the treatment of certain types of arthritis. Anti-TNF medications, such as infliximab and etanercept, have shown impressive efficacy in reducing inflammation, improving symptoms, and slowing disease progression. These therapies have provided new hope for individuals with arthritis, particularly those who do not respond well to conventional treatments.
Impact of TNF gene polymorphisms on treatment response
Genetic variations in the TNF gene can influence an individual’s response to anti-TNF therapies. Certain gene variants have been associated with a better response to treatment, while others may be linked to a reduced or no response. Understanding the impact of TNF gene polymorphisms on treatment response can help tailor therapy choices for optimal outcomes in arthritis patients.
Conclusion
In conclusion, genetic factors play a crucial role in the development of arthritis. Certain genetic variations and mutations can increase an individual’s susceptibility to different types of arthritis. Research has identified specific genetic factors associated with arthritis, such as HLA genes, PTPN22 gene, IL6 gene, IL1B gene, and TNF gene. Understanding the role of these genes in arthritis provides insights into disease mechanisms, helps predict disease outcomes, and offers potential targets for personalized medicine. Genetic research in arthritis holds tremendous promise in improving diagnosis, treatment, and overall management of this chronic and often debilitating condition. By unraveling the genetic factors linked to arthritis development, we can pave the way for more effective and individualized therapeutic strategies.
We have more great information on the subject of Arthritis HERE

